Nail fungus is a common issue that can make nails look yellow, thick, and brittle. It often starts slowly and worsens without treatment. To cure nail fungus, people typically need antifungal treatments such as creams, oral medications, or laser therapy, depending on the severity and type of fungus involved.
Diagnosing the exact cause is important because other conditions can look like nail fungus. A healthcare provider may take nail clippings to confirm the infection before recommending the best treatment plan. While some home remedies exist, medically approved treatments are usually more effective and faster at clearing the infection.
Getting rid of nail fungus requires patience since treatment can take several months. Lifestyle changes and good nail care help prevent the fungus from coming back after treatment is finished.
Key Takeways
- Nail fungus requires targeted antifungal treatments for effective cure.
- Accurate diagnosis helps ensure the right treatment is used.
- Ongoing nail care is important to prevent recurrence.
Understanding Nail Fungus
Nail fungus affects the toenails and fingernails by causing changes in color, texture, and thickness. It develops from fungal organisms that invade the nail and surrounding skin. Knowing what nail fungus is, the types of infections, and how it spreads helps in managing and preventing it effectively.
What Is Nail Fungus
Nail fungus, also called onychomycosis, is an infection caused by fungi entering the nail through small cracks or cuts. It often starts as a white or yellow spot under the nail edge and gradually affects the whole nail. The infected nail may thicken, become brittle, or even emit an unpleasant smell.
This condition is more common in toenails than fingernails. It thrives in warm, moist environments, which is why it often appears in people who wear closed shoes or have sweaty feet. Nail fungus can persist and worsen without proper care or treatment.
Common Types of Nail Fungal Infections
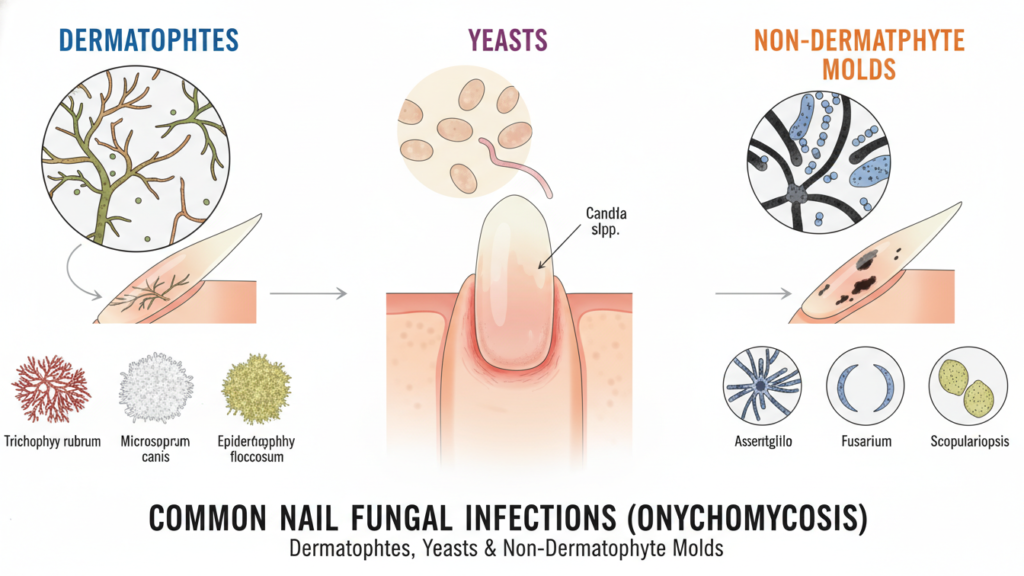
Fungal infections that affect nails are mainly caused by three groups: dermatophytes, yeasts, and non-dermatophyte molds.
- Dermatophytes are the most common cause. They feed on keratin, the protein in nails.
- Yeasts like Candida can infect nails, especially fingernails, often in people with weakened immunity.
- Non-dermatophyte molds are less common but can cause infections, often after nail injury.
Symptoms may vary depending on the type of fungus but usually involve nail discoloration, thickening, and crumbling edges. Knowing the cause helps doctors choose the right treatment.
How Nail Fungus Spreads
Nail fungus spreads through direct contact with fungal spores. These spores live in warm, damp areas like locker rooms, swimming pools, and dirty socks or shoes. Sharing nail clippers or walking barefoot in public places can increase the risk.
The infection can also spread from one nail to others or from skin to nail. People with weakened immune systems, diabetes, or poor circulation are more vulnerable. Keeping feet dry, practicing good hygiene, and avoiding shared personal items help reduce the chance of spread.
Symptoms and Diagnosis of Nail Fungus
Nail fungus causes visible changes in the nail’s color, texture, and shape. Identifying early signs helps start treatment sooner. Accurate diagnosis often requires professional testing because other conditions can look like fungal infections.
Identifying Early Signs
Nail fungus usually begins with small changes in the nail’s appearance. The affected nail might become yellow, white, or brown. It can start as a white or yellow spot under the tip of the nail. Over time, the nail may become thicker, brittle, or crumbly.
Other signs include nails looking distorted or misshapen. The nail might also develop a foul smell. Discomfort or pain can occur when pressing on the nail or wearing shoes. Early identification is important because the infection can spread to other nails or skin if left untreated.
When to Seek Medical Advice
A person should see a healthcare provider if the nail changes worsen or do not improve after home care. Seeking advice is important when nails become painful, thick, or show color changes. It is also necessary if the nail looks infected with redness or pus.
People with diabetes, weakened immune systems, or poor circulation should get prompt medical attention for nail problems. These groups are at higher risk for complications from nail fungus. Early treatment can prevent more serious infections and nail damage.
Diagnostic Methods
Doctors start diagnosis by examining the nails for visible signs like thickening or discoloration. They may collect nail clippings or scrape under the nail to get samples.
These samples go to a lab for testing to find the exact organism causing the problem. Tests can identify if it’s a fungus, yeast, or bacteria since other conditions like psoriasis can look similar.
| Diagnostic Step | Purpose |
|---|---|
| Visual Nail Exam | Spot signs of fungus, damage |
| Nail Clippings/Scrapings | Collect samples for lab analysis |
| Lab Culture or Microscopy | Confirm type of infection |
Lab results guide the most effective treatment method for the specific infection.
Effective Treatment Options

Nail fungus can be treated with several methods that target the infection directly. These include medicines applied to the nail, pills taken by mouth, and advanced light therapies. Each option has specific uses, benefits, and timeframes for results.
Topical Antifungal Medications
Topical antifungal treatments are creams, ointments, or medicated nail lacquers applied directly to the infected nail and skin around it. These products usually contain ingredients like ciclopirox or amorolfine.
They work best for mild to moderate infections or when the fungus affects only part of the nail. Continuous daily use is essential and treatment can last from several weeks to months. Many topical medicines require filing the nail surface for better absorption.
Topicals have fewer side effects compared to oral medications since they remain mostly outside the body. However, they may not fully cure severe cases because the fungus can be deep under the nail plate.
Oral Antifungal Medications
Oral antifungal medicines are pills usually prescribed for more stubborn or widespread nail fungus. Common drugs include terbinafine and itraconazole.
These medications work from the inside by helping new healthy nails grow and replacing the infected ones. Treatment length is typically 6 to 12 weeks but it may take several months to see improvement.
Oral antifungals can be more effective than topical treatments because they reach the fungus at its source. However, they can cause side effects like liver problems or skin rash, so doctors monitor patients with blood tests during treatment.
Laser Therapy
Laser therapy uses concentrated light to target and destroy fungal cells under the nail without harming surrounding skin. This FDA-approved method offers an alternative for those who cannot use medications.
The procedure is painless, done in sessions lasting about 30 minutes. Patients may need multiple sessions over several weeks. Laser therapy often speeds up nail clearing compared to other treatments.
While laser treatment can reduce the fungus, evidence about its long-term cure rates is still limited. It is usually more costly and less commonly covered by insurance but is considered safe when performed by professionals.
Natural and Home Remedies
Several home treatments can help reduce nail fungus. These include using certain oils, soaking nails in vinegar, and applying baking soda. Each method has specific ways to use it and varying levels of effectiveness.
Essential Oils
Essential oils like tea tree, lavender, and oregano are popular for treating nail fungus. They have natural antifungal and antiseptic properties. Tea tree oil is especially well-known for fighting fungus.
To use essential oils, one should dilute them with a carrier oil, such as coconut or olive oil. Applying this mix to the affected nail twice daily can help reduce fungus over time. Consistency is important because results may take weeks or months.
Some people may experience skin irritation, so it is advised to test a small area before full use. Essential oils should never be ingested and should be kept away from eyes.
| Essential Oil | Properties | Usage Tip |
|---|---|---|
| Tea Tree Oil | Antifungal, antiseptic | Dilute, apply twice daily |
| Lavender Oil | Antifungal, soothing | Helps reduce inflammation |
| Oregano Oil | Strong antifungal | Use carefully, dilute well |
Vinegar Soaks
Vinegar, especially apple cider vinegar, has acid that may slow fungal growth. Soaking nails in a vinegar and water mix creates an environment where fungus struggles to survive.
The usual ratio is 1 part vinegar to 2 parts warm water. Soaking for 15 to 20 minutes daily can help. After soaking, nails should be dried thoroughly to prevent more fungal growth.
Vinegar soaks are safe for most people, but the smell might be strong. It is helpful to use this treatment alongside other remedies for better results.
| Vinegar Type | Dilution Ratio | Soak Time |
|---|---|---|
| Apple Cider Vinegar | 1 part vinegar, 2 parts water | 15-20 minutes daily |
| White Vinegar | Same as above | Similar effects, less odor |
Baking Soda Treatments
Baking soda can neutralize odor and create a less favorable surface for fungus. It absorbs moisture, which fungi need to grow.
One way to use baking soda is making a paste with water and applying it directly to the nail. Leave it on for 10 minutes, then rinse off and dry fully. Another method is sprinkling baking soda inside shoes or socks to reduce fungal growth.
Baking soda is gentle and often safe but may need to be combined with other treatments for best results.
| Method | Instructions | Benefits |
|---|---|---|
| Paste Application | Mix with water, apply to nail for 10 minutes | Reduces moisture, mild antifungal effect |
| Sprinkle in Shoes | Sprinkle inside shoes or socks daily | Helps prevent fungus in footwear |
Preventing Recurrence of Nail Fungus

Stopping nail fungus from coming back requires careful attention to daily habits, the environments nails are exposed to, and the items worn on the feet. Consistent care helps maintain healthy nails and lowers the chance of reinfection.
Hygiene Tips
Keeping nails clean and dry is essential. People should wash their feet daily and dry them thoroughly, especially between the toes. Moist environments encourage fungal growth, so using a clean towel and changing it often reduces risk.
Nail trimming should be done regularly with sanitized tools. Cutting nails short helps prevent fungus spread, but care must be taken to avoid injuring the skin around the nails. Avoid sharing nail clippers or files with others.
Applying antifungal powders or sprays on feet can help keep fungus away. It is also important to disinfect nail care tools after each use. Keeping strong habits around hygiene lowers the chance that fungus returns.
Protecting Nails in Public Spaces
Fungal infections often begin in warm, moist areas like pools, locker rooms, and showers. Wearing waterproof sandals or flip-flops in these places reduces direct contact with contaminated surfaces.
People should avoid walking barefoot on public floors to prevent exposure to fungal spores. If using public showers, drying feet immediately afterward is important to keep the environment dry.
Carrying personal towels and avoiding shared nail care equipment in public settings further protects nails. These simple actions help block common ways that nail fungus reappears.
Footwear and Sock Choices
Fungus grows best in dark, damp shoes. Discarding old, infected shoes is necessary to avoid reinfection. Shoes made of breathable material allow air circulation, keeping feet dry.
Socks should be made from moisture-wicking fabrics like cotton or wool. They should be changed daily, or more often if feet sweat a lot. Tight shoes that squeeze the toes can trap moisture and make fungus more likely.
Rotating footwear gives shoes time to dry between uses. Using antifungal sprays or powders inside shoes adds protection. Paying attention to footwear and socks is key to stopping nail fungus from returning.
Risks and Complications
Nail fungus treatments can sometimes cause side effects that affect skin or overall health. On the other hand, leaving nail fungus untreated can lead to serious problems, especially for people with other health issues. Understanding these risks helps in making safer choices for treatment and care.
Potential Side Effects of Treatments
Common treatments for nail fungus include antifungal creams, oral medications, and laser therapy. Oral antifungal drugs may cause side effects such as upset stomach, headache, or skin rash. In some cases, they can affect the liver, so doctors often monitor liver function during treatment.
Topical treatments like creams can cause redness, itching, or irritation at the application site. Laser therapy is generally safe but may cause minor pain or redness after the procedure.
Patients with other health conditions or those taking certain medicines should consult their doctors before starting treatment because drug interactions or allergies can increase risks.
Complications from Untreated Nail Fungus
If nail fungus is not treated, the infection can worsen and spread to other nails or skin areas like between toes (athlete’s foot). The nail may become thick, brittle, and painful, making walking or wearing shoes uncomfortable.
In people with diabetes, poor immunity, or circulation problems, untreated nail fungus can lead to severe complications. These include skin ulcers or bacterial infections that might need antibiotics or even surgery.
In rare cases, untreated nail fungus might cause permanent nail damage or increase the risk of more serious foot problems, including amputation in extreme cases. Early diagnosis and treatment reduce these risks significantly.
When to Consult a Specialist
If nail fungus does not improve after using over-the-counter treatments, it is time to see a specialist. Persistent symptoms or worsening conditions need professional attention to prevent further damage.
A dermatologist is the best doctor to consult for nail fungus. They specialize in skin and nail conditions and can provide an accurate diagnosis. This often involves taking nail clippings or using a microscope to identify the specific fungus.
People should also see a specialist if their nails become very thick, brittle, or painful. Severe infections can cause permanent nail damage or spread to other nails. A doctor can offer stronger treatments like oral antifungal drugs or laser therapy.
Those with other health conditions, such as diabetes or a weakened immune system, should consult a doctor sooner. These conditions can make nail fungus harder to treat and increase the risk of complications.
Here are signs to see a specialist:
- No improvement after several weeks of home treatment
- Thickened or crumbling nails
- Pain or discomfort in the nail or surrounding skin
- Underlying health issues that affect healing
A specialist will create a treatment plan based on the type of fungus, the extent of the infection, and the patient’s health. Early consultation improves the chances of successful treatment.
Long-Term Nail Care After Treatment
Proper care after treating nail fungus is essential to keep nails healthy and to reduce the chance of the fungus returning. This includes regular cleaning, using the right products, and watching for early signs if the infection starts again.
Maintaining Nail Health
Keeping nails clean and dry is vital to support healing and prevent fungal growth. He or she should wash feet daily with soap and water, then dry thoroughly, especially between the toes. Wearing shoes made of breathable materials helps reduce moisture buildup.
Using antifungal powders or sprays can protect the nails from reinfection. It is also important to trim nails straight across and keep them short to avoid damage. Avoid sharing nail clippers or shoes with others to limit the spread of fungus.
Regularly changing socks, especially after heavy sweating, and avoiding walking barefoot in public places like locker rooms or pools further lowers the risk. Good foot hygiene supports stronger, healthier nails after treatment.
Monitoring for Signs of Recurrence
Early detection of nail fungus returning is critical to address it quickly. Signs such as nail thickening, discoloration, brittleness, or crumbling should not be ignored.
He or she should inspect nails weekly or monthly and note any changes in texture or color. If symptoms appear, prompt consultation with a healthcare provider is advisable for early treatment.
Tracking progress with photos can help compare changes over time. Taking action early when symptoms arise often leads to quicker control, reducing the severity and spread of the infection.
Lifestyle Changes to Support Recovery
Making some changes in nutrition and daily habits can help the body fight nail fungus more effectively. Paying attention to what is eaten and how nails are cared for can speed up healing and prevent the fungus from returning.
Nutrition and Immune Support
A balanced diet plays an important role in fighting nail fungus. Reducing sugar and simple carbs helps because fungi feed on these. Instead, adding foods rich in vitamins C, E, and zinc can boost the immune system. These nutrients help the body fight infections and repair damaged tissue.
Drinking plenty of water keeps the skin and nails hydrated, which supports healing. Probiotic foods like yogurt or fermented vegetables may also improve gut health. A stronger immune system can prevent fungus from growing back.
Avoiding excessive processed foods and junk food is important. These can weaken immune response and slow recovery. A diet focused on whole, natural foods offers the best support.
Daily Routines for Healthy Nails

Keeping feet clean and dry is essential to stop fungus from spreading. Washing feet daily with soap, drying thoroughly, and changing socks often creates an environment that is unfriendly to fungal growth.
Wearing breathable shoes and moisture-wicking socks like cotton or bamboo helps keep nails dry. Avoid sharing nail tools or wearing tight shoes that can damage the nail or skin.
Regularly trimming nails straight across helps prevent damage. Avoiding artificial nails and harsh nail polish during treatment allows nails to grow back healthier.
Using antifungal powders or sprays in shoes can reduce fungal spores. Consistent foot care routines improve treatment results and reduce the chance of reinfection.
FAQS
Does nail fungus go away on its own?
Nail fungus rarely clears up without treatment. It often lasts a long time and can spread to other nails or skin. Treatment is usually needed to fully remove the infection.
How long does it take to cure nail fungus?
Most treatments take weeks or even months. Nails grow slowly, so visible improvement may take time. Persistence and following a treatment plan are important.
Can nail fungus be treated at home?
Some home remedies may relieve symptoms but are not always effective. Medical treatments like antifungal creams, oral drugs, or laser therapy work better for stubborn cases.
Is there a quick fix to kill nail fungus?
No treatment cures nail fungus instantly. Even faster methods, such as laser therapy, require several sessions over weeks. Patience is necessary for full recovery.
When should someone see a doctor?
If the infection is painful, spreading, or not improving after self-care, consulting a healthcare provider is advised. They can recommend the right treatment based on the fungus type and severity.
Can nail fungus come back?
Yes, nail fungus can return after treatment. Preventive steps like keeping nails clean and dry help reduce the chance of reinfection.
| Question | Quick Answer |
|---|---|
| Does it clear without help? | Rarely, usually needs treatment |
| How long for visible results? | Weeks to months |
| Are home remedies effective? | Sometimes, but medical treatment is better |
| Any instant cures? | No, require weeks of treatment |
| When to see a doctor? | If pain, spread, or no improvement |
Conclusion
Treating nail fungus takes time and patience. The choice of treatment depends on the severity of the infection and the patient’s overall health.
Oral medications usually work the fastest but may not be suitable for everyone. Topical creams, ointments, and home remedies often require consistent use over months. Laser therapy is another option that targets the fungus directly and can speed up the healing process.
Proper nail care is important during treatment. Regular trimming and filing help remove infected nail material. This also prevents the fungus from spreading or getting worse.
Patients should follow their healthcare provider’s advice closely. Treatment plans are often tailored based on how much the nail is affected and the type of fungus involved.
Key points to remember:
- Nail fungus treatment may take several months.
- Oral, topical, and laser treatments are common options.
- Keeping nails clean and trimmed supports healing.
- Consistency and patience improve success rates.
Managing expectations helps people stay motivated to continue treatment until nails look healthy again.

